What are Infected Wounds?
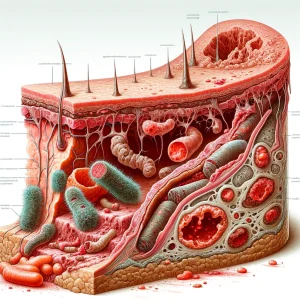
An infected wound is a localized medical complication that occurs when a break in the skin is successfully invaded by pathogenic microbes. Instead of being eliminated by the body’s immune system, these germs begin to multiply within the damaged tissue. This proliferation triggers a significant inflammatory response, which is the direct source of the classic signs of infection like increased pain, swelling, and pus formation.
It is important to distinguish between contamination and true infection. Virtually all wounds are contaminated, meaning they contain some bacteria from the environment or surrounding skin. An infection develops only when these microbes overcome the local immune defenses, either due to a large number of invading bacteria, their high virulence (aggressiveness), or a weakened state in the host. This process can happen in any type of wound, from a minor scrape to a deep surgical incision or a chronic ulcer.
Causes:- Heavy Microbial Contamination: The initial introduction of a large number of bacteria is a primary driver. These microbes can originate from the object that caused the injury (e.g., soil on a tool), the surrounding environment, or even the person's own skin flora being driven deep into the tissue.
- Presence of Foreign Debris: Any foreign material—such as dirt, glass shards, or splinters—that remains embedded in a wound can act as a breeding ground for bacteria. This debris provides a surface for microbes to attach to and shields them from the body's immune cells.
- Retention of Devitalized (Necrotic) Tissue: Tissue that has lost its blood supply and died as a result of the injury is known as necrotic tissue. It cannot be defended by the immune system and serves as a rich nutrient source for bacterial growth, essentially fueling the infection.
- Compromised Blood Supply to the Area: Effective healing and defense require robust blood circulation to deliver oxygen and immune cells to the wound bed. Any condition that diminishes this supply, such as severe swelling or underlying peripheral vascular disease, cripples the local immune response and allows bacteria to multiply unchecked.
- A Person's Underlying Health Status: The risk is markedly higher for those with chronic conditions that impair blood flow, such as peripheral artery disease or poorly controlled diabetes. Inadequate circulation deprives the wound site of the oxygen and immune cells essential for fighting off microbial invaders.
- Individuals with Suppressed Immune Function: A weakened immune system presents a significant vulnerability. This includes patients taking immunosuppressant drugs after an organ transplant, those undergoing chemotherapy, or people living with conditions like HIV. Their bodies cannot mount a sufficiently powerful response to contain a bacterial assault.
- The Characteristics of the Injury Itself: Some wounds are inherently more prone to infection. Deep puncture wounds, bites from animals or humans, and injuries that retain foreign debris or dead tissue create an ideal, protected environment for bacteria to multiply.
- Advanced Age: The elderly population faces an elevated risk. They often have thinner, more fragile skin that tears easily, which can be combined with a naturally less vigorous immune response and a higher likelihood of having circulatory issues, creating a convergence of vulnerabilities.