What is Omphalitis?
Omphalitis is an infection of the navel area that occurs specifically in the first few weeks of a baby’s life. It involves the umbilical stump—the small piece of tissue that remains after the umbilical cord is clamped and cut—and the ring of skin at its base. The umbilical stump itself is non-living tissue that is meant to dry up and separate from the body naturally. An infection takes hold when bacteria move beyond this dying tissue and invade the living skin and underlying abdominal wall at the point of attachment.
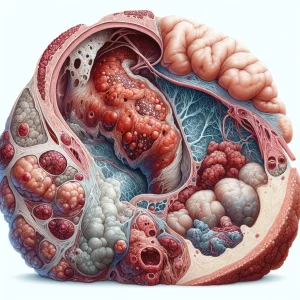
The condition is identified by signs of an active infection spreading out from the base of the stump. This includes a distinct area of redness and warmth on the belly, swelling of the navel tissue, and often a foul-smelling, cloudy, or yellowish discharge. Unlike the minor crusting or a few drops of blood that can be part of normal healing, omphalitis represents a true bacterial cellulitis, or skin infection, in this uniquely vulnerable area of a newborn.
Causes:- A Gateway for Microbial Entry: The umbilical stump is essentially a wound in the process of healing. This area of devitalized, or dying, tissue provides a direct, temporary pathway for bacteria on the skin surface to bypass the infant's primary physical defense barrier.
- Colonization of the Umbilical Stump: The infection is initiated when common bacteria take up residence on this non-living tissue. Organisms like Staphylococcus aureus, group A Streptococcus, or Gram-negative bacteria such as Escherichia coli can be transferred from caregivers' hands or the surrounding environment, where they multiply rapidly in the moist, nutrient-rich stump.
- Invasion into the Abdominal Wall: The actual disease begins when these proliferating bacteria migrate from the non-living stump into the viable, living tissue of the baby's abdominal wall. This invasive step triggers an aggressive inflammatory response from the infant's immune system, resulting in the characteristic redness, swelling, and pus formation.
- Premature or Low-Birth-Weight Infants: Babies born before full term or with a lower than average weight have less-developed host defenses. Their immune systems are not yet fully matured, and their skin is often thinner, providing a less effective physical barrier against bacterial invasion.
- Complications During Labor and Delivery: A prolonged period between the rupture of the maternal membranes (water breaking) and the baby's delivery can increase exposure to vaginal bacteria. Similarly, an active maternal infection around the time of birth can lead to the infant being colonized with pathogenic organisms.
- Use of an Umbilical Catheter: Newborns, particularly in a neonatal intensive care unit (NICU), may require a catheter to be placed in a blood vessel of the umbilical stump for medication or monitoring. This device, while medically necessary, creates a direct pathway for bacteria to bypass the skin and enter the body.
- Non-Sterile Birthing Conditions: Infants delivered in environments where strict aseptic techniques are not followed face a higher risk. Contamination of the umbilical cord with bacteria from the environment or non-sterile hands during or immediately after the birthing process increases the likelihood of infection.
- Improper Stump Care: Deviating from modern medical advice to keep the umbilical stump clean and dry can increase risk. Applying unsterile substances, powders, or traditional dressings to the stump can introduce a heavy load of bacteria and trap moisture, creating an ideal environment for them to multiply.