What is Psoriasis?
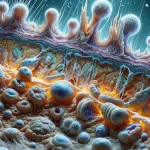
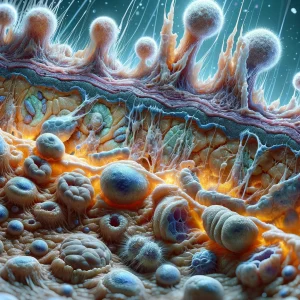
Psoriasis is the physical manifestation of a misdirected immune system. In this condition, the body’s own defense mechanisms incorrectly identify healthy skin cells as a threat that needs to be eliminated. In response to this mistaken alarm, the immune system unleashes a cascade of inflammatory signals that command the skin to overproduce new cells at an extreme rate. A process that should normally span several weeks for a skin cell to mature and be shed is compressed into a matter of mere days.
This rapid proliferation prevents the skin from shedding the excess cells properly, forcing them to accumulate on the surface. This pile-up results in the development of well-defined, raised areas known as plaques. These plaques typically appear as reddened skin due to increased blood flow from the inflammation, and are often covered by silvery-white scales composed of the dead, built-up skin cells. While plaque psoriasis is the most prevalent form, other variations exist, such as guttate psoriasis, which appears as small, drop-like spots, and pustular psoriasis, characterized by pus-filled blisters.
Causes:- A Faulty Genetic Blueprint: The foundational cause of psoriasis is an inherited predisposition. Individuals carry specific genes that fundamentally alter how their immune system is programmed to behave. This genetic inheritance creates a lifelong potential for the immune system to launch an inappropriate, inflammatory assault on the body's own skin cells.
- Activation by a Triggering Event: The condition typically remains dormant until an external or internal factor sets the faulty immune response in motion. This trigger event acts like a switch that turns the disease on. Well-known triggers include a significant infection (such as strep throat), an injury to the skin (a phenomenon known as the Koebner response), periods of intense psychological stress, or taking certain systemic medications.
- Having a Family History: The single greatest predictor for developing psoriasis is genetics. If a person's parents or siblings have the condition, it signifies that they have likely inherited the specific immune system characteristics that can lead to the disease.
- Tobacco Use: Smoking not only elevates the initial risk of developing psoriasis but is also strongly correlated with more severe and widespread forms of the disease. The toxins in tobacco are thought to promote the specific type of inflammation that drives psoriasis flare-ups.
- Obesity: Individuals with obesity are at a markedly higher risk for psoriasis. Fat tissue is metabolically active and produces inflammatory chemicals that can contribute to the systemic inflammation that underpins the development and persistence of psoriatic plaques.
- High Levels of Chronic Stress: People who experience sustained, high levels of psychological stress have a greater susceptibility. Chronic stress disrupts the body's hormonal balance and immune regulation, which can create an internal environment that is conducive to activating the disease.