Key Facts
- A prostatectomy means we’re removing the entire prostate gland to get rid of the cancer. That’s the mission.
- Initial healing takes about six weeks, but getting back to “normal” with urinary and sexual function can take a year or more. It’s a marathon.
- Most surgeries today use a robot. This gives us a magnified 3D view and incredible precision around delicate nerves.
- Let’s be blunt: urinary leaks and erectile dysfunction are the biggest hurdles. We have plans to manage both.
- More than the technology, the experience of your surgeon is what truly counts.
On This Page:
What Is a Prostatectomy, Really?
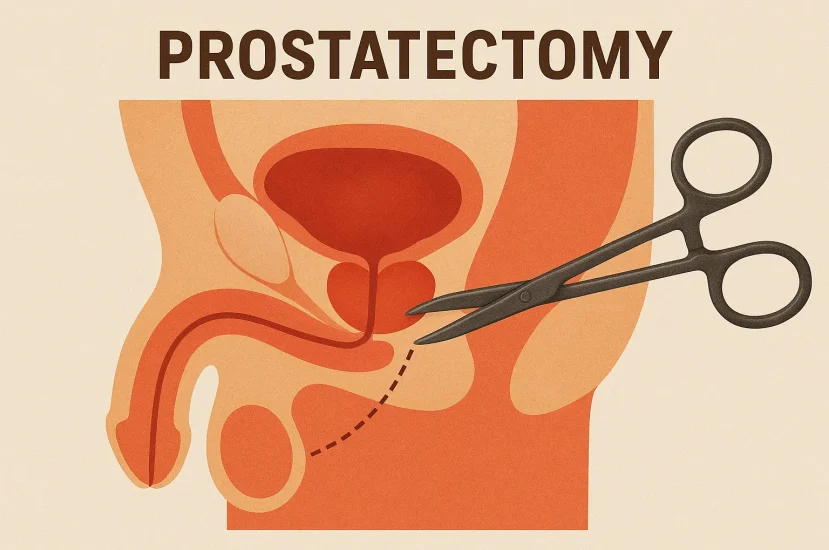
Look, no man wants to be having this conversation. I know that. When I tell you that you need your prostate out, the questions start flooding in. So let’s just cut to the chase. A prostatectomy is an operation to remove your prostate gland. We do it for one reason: to get the cancer out of your body, hopefully for good.
The prostate isn’t in an easy-to-reach spot. It’s tucked deep in the pelvis, surrounded by your bladder and rectum. More importantly, it’s wrapped in a web of nerves and blood vessels that control two things you care a lot about: staying dry and getting an erection. My job is to perform a clean eviction of the prostate while doing as little damage to the neighborhood as possible.
Robot vs. Scalpel: Does It Matter?
The first thing everyone asks is about the robot. Is it better? The short answer is: the person driving the robot matters more than the robot itself. But the technology is impressive, and it’s what we use for most cases today.
| The Method | How It Works | The Bottom Line |
|---|---|---|
| Open Surgery | This is the classic approach. One incision in the lower belly. My hands are directly on the tissue. It’s a reliable method I’ve used for years. | Sometimes, this is the better route if you’ve got a lot of scar tissue from past operations. |
| Robotic-Assisted Surgery | I sit at a console and control robotic arms through a few small punctures in your abdomen. It gives me a 3D, high-definition view, and the instruments have more flexibility than a human wrist. | This is the standard now. That precision helps immensely when I’m trying to peel those paper-thin erection nerves off the prostate. |
Ultimately, find a surgeon who has done hundreds, if not thousands, of these operations. That’s your best bet, regardless of the tool.
The Tough Questions: Leaks and Sex
Alright, let’s talk about the two things you’re actually worried about. Forget the surgical risks of bleeding and infection—they’re low. This is about your quality of life afterward.
Urinary Leaks (Incontinence)
After the surgery, when we take the catheter out, you are going to leak. I tell every single patient this. Don’t panic. It’s normal. Your body’s plumbing has been rerouted, and the new system needs to learn how to work. For almost everyone, it gets better. But it takes time and work. Your best weapon? Kegel exercises. Start them now.
Erections (ED)
This is the hardest part of the recovery for many men. The nerves that control erections are unbelievably delicate. Imagine trying to peel wet tissue paper off an orange without tearing it. That’s what we’re up against. Even with a perfect nerve-sparing surgery, those nerves get bruised and go into shock. Waking them up is a slow process—it can take 18 months or more. We have a whole playbook for ED after prostate cancer treatment, from pills like Cialis to other therapies. We will get you through it, but it requires patience.
Your Homework Before Surgery
You have a job to do before you ever get to the operating room. Think of this as training for the main event.
- Master the Kegel: I’m saying it again because it’s that important. Learn to isolate and squeeze your pelvic floor muscles. It will pay off.
- Get Your Body Ready: We’ll do a full medical check-up. Stop any blood thinners as instructed. Eat well. Don’t smoke.
- The Bowel Prep: Nobody likes it, but cleaning out your system the day before is a non-negotiable safety measure. Just get it done.
The Road Back: A Realistic Recovery Timeline
Recovery isn’t a straight line. There will be good days and bad days.
- First 24 Hours: You’ll be in the hospital, feeling tired and sore. You’ll have a catheter. Our goal is simple: manage your pain and get you on your feet for a short walk.
- First Week Home: You and your new friend, the catheter. Your main jobs are to walk a little every day, drink plenty of water, and avoid any heavy lifting. Seriously, don’t even lift a gallon of milk.
- 1-3 Months Post-Op: The catheter is gone. Now the real work on bladder control begins. You’ll likely wear pads. You’ll see gradual progress. You’ll start feeling more like yourself and can get back to most normal activities.
- Up to 18 Months: This is the long haul. Urinary control should be much, much better. Now, the focus really shifts to sexual rehabilitation. We’ll be working closely together on a plan to restore function. Be persistent. Don’t give up.
This is a major life event. But it’s a solvable problem. My advice? Be an active participant in your own care. Ask hard questions. And know that you have a team in your corner every step of the way.