What is a Headache?
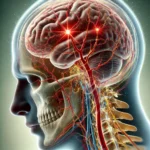
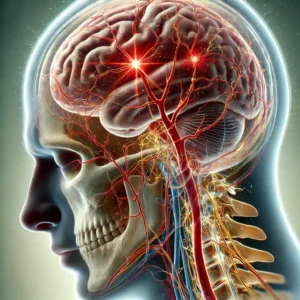
A headache is a pain or discomfort in the head, scalp, or neck. It is one of the most prevalent medical complaints and can significantly impact daily life. Headaches are broadly categorized into two groups: primary and secondary.
Description of the Condition
Primary headaches are independent conditions caused by overactivity of, or problems with, pain-sensitive structures in the head. They are not a symptom of an underlying disease. The most common types include tension-type headache, migraine, and cluster headache.
Secondary headaches are symptoms of another health disorder that activates the pain-sensitive nerves of the head. Numerous conditions can cause them, ranging from dehydration and sinus infections to more serious issues like hypertension, meningitis, or stroke. Identifying whether a headache is primary or secondary is a crucial step in diagnosis.
Causes:- Neurological and Vascular Dysfunction: Primary headaches like migraines are linked to abnormal brain activity affecting nerve signals, chemicals, and blood vessels. Tension-type headaches are associated with muscle contraction and heightened pain sensitivity.
- Underlying Medical Condition: The headache is a direct symptom of another issue. Common causes include hypertension, acute sinusitis, medication overuse, dehydration, and eye strain.
- Medication-Overuse Headache (MOH): Also known as rebound headache, this is a secondary headache caused by frequent, excessive use of pain-relief medication (like NSAIDs or triptans) for treating headache episodes. Paradoxically, the medication itself begins to trigger headaches.
- Family History: A family history of migraines, in particular, is a strong risk factor, suggesting a genetic component to the condition.
- Stress and Poor Sleep: High stress levels, anxiety, irregular sleep patterns, and poor sleep quality are major triggers for tension-type headaches and migraines. Resources on managing anxiety may be relevant.
- Use of Certain Medications: Regular use of pain relievers can lead to Medication-Overuse Headache (MOH). Additionally, some drugs, such as vasodilators used for erectile dysfunction, are known to cause headaches as a side effect. Information on this can be found in a urologist's guide to ED pill side effects.