What is Hypopituitarism?
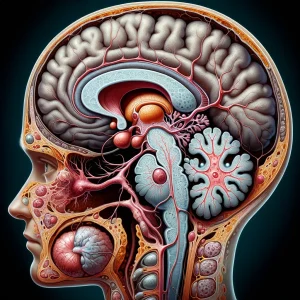
Hypopituitarism is a condition of glandular failure originating in the pituitary, a small, pea-sized structure located at the base of the brain. This gland serves as the primary regulator of the body’s entire endocrine network, acting as a master control center. Its role is to produce and dispatch crucial signaling hormones—such as thyroid-stimulating hormone (TSH), growth hormone (GH), and adrenocorticotropic hormone (ACTH)—which instruct other glands like the thyroid and adrenals on when to perform their functions. When the pituitary underproduces, these downstream glands do not receive their necessary commands, leading to a cascade of hormonal deficits. The condition can involve a shortage of a single hormone or, in the case of panhypopituitarism, a complete or near-complete failure of all pituitary hormone production.
Causes:- Physical Compression and Surgical Impact: The most common trigger is the physical presence of a tumor, either within the pituitary itself or in a nearby brain region. As a non-cancerous (benign) or cancerous growth expands, it exerts direct physical pressure on the delicate hormone-producing cells, disrupting their function and blood supply. Furthermore, the very medical procedures required to remove such growths, including intricate neurosurgery, can unavoidably cause scarring or damage to the gland's tissue.
- Destruction from Therapeutic Radiation: The pituitary gland is highly sensitive to therapeutic radiation directed at the head or brain, often used to treat cancers. The high-energy beams, while targeting malignant cells, can inflict cumulative and irreversible damage on the pituitary's hormone-secreting cells. This process can be gradual, with the gland's functional capacity diminishing over a period of months or even years following the conclusion of radiation treatment.
- Sudden Interruption of Blood Supply: A catastrophic disruption of blood flow to the pituitary can cause a large number of its cells to die, an event known as infarction. This can be triggered by severe blood loss and a drop in blood pressure elsewhere in the body (such as during major trauma or complicated childbirth) or by spontaneous bleeding directly into the pituitary gland. Without a constant supply of oxygen-rich blood, the glandular tissue cannot survive, leading to an abrupt failure in hormone production.
- Individuals with a History of Brain Tumors: People who have been diagnosed with tumors of the pituitary gland (adenomas) or nearby structures like the hypothalamus are at the highest risk. The risk stems from both the physical pressure of the tumor itself and the potential for glandular damage during its surgical removal.
- Patients Who Have Undergone Head or Neck Radiation: A person who has received radiation therapy for cancers of the brain, nasopharynx, or as part of total body irradiation for leukemia has a significant risk. The pituitary gland is highly sensitive to radiation, and its function can decline months or even years after the treatment has concluded.
- Survivors of Traumatic Brain Injury (TBI): Individuals who have experienced a severe head injury, such as from a motor vehicle accident or a significant fall, are vulnerable. The physical impact can directly damage the pituitary or disrupt the delicate stalk connecting it to the hypothalamus, interrupting crucial signals and blood flow.
- People with Specific Vascular Events: This includes individuals who have had a stroke affecting the pituitary's blood supply or women who suffered from extreme blood loss and circulatory shock during childbirth, a condition known as Sheehan's syndrome.