What is Listeriosis?
The illness known as listeriosis originates from the bacterium Listeria monocytogenes, an organism uniquely adapted to survive in various environments, including refrigerated temperatures. Listeriosis manifests in two principal forms. The first is a non-invasive gastrointestinal illness, which remains confined to the gut and produces symptoms similar to common food poisoning.
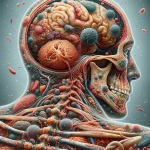
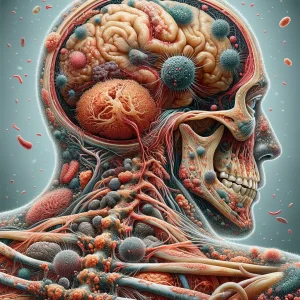
The second, and far more dangerous, form is invasive listeriosis. In this state, the bacteria breach the intestinal wall, enter the bloodstream, and spread throughout the body. This systemic infection can cross protective physiological barriers, allowing it to target the central nervous system, where it can cause meningitis or encephalitis. In pregnant individuals, the bacteria can cross the placental barrier, leading to infection of the fetus, which can result in miscarriage, stillbirth, or severe illness in the newborn.
Causes:- Environmental Persistence of the Bacterium: The ultimate origin is the bacterium Listeria monocytogenes itself, which is a hardy and widespread organism. It naturally resides in soil, decaying vegetation, and water, and can be carried in the intestinal tracts of various animals, creating a vast and persistent reservoir in nature.
- Introduction into the Food Chain: Contamination is the critical step that introduces the bacterium to humans. This can happen at the farm level when raw produce comes into contact with contaminated soil or water, or within a food processing facility where the organism can establish itself and form biofilms on equipment, leading to the contamination of ready-to-eat products like deli meats, soft cheeses, and packaged salads.
- Oral Ingestion of the Pathogen: The infection is initiated when an individual consumes a food product carrying a sufficient quantity of Listeria. A key part of its causal mechanism is its ability to survive the highly acidic environment of the stomach, a barrier that eliminates many other types of bacteria, allowing it to pass into the intestines unharmed.
- Penetration of the Intestinal Barrier: Once in the intestines, Listeria actively triggers its own engulfment by the cells lining the intestinal wall. After it is inside these host cells, it uses the cell's own structural components to propel itself into neighboring cells, effectively breaching the intestinal barrier and gaining direct access to the bloodstream, which then allows it to spread systemically.
- Pregnant Individuals and Their Newborns: This group is uniquely susceptible. A pregnant person may only experience a mild, flu-like illness, but the Listeria bacteria can cross the placenta and infect the developing fetus, potentially causing life-threatening complications for the baby.
- Adults Aged 65 and Older: The natural decline of the immune system's effectiveness that occurs with aging makes older adults less capable of fighting off an initial Listeria exposure, allowing the infection to more easily become invasive.
- Individuals with Compromised Immune Systems: Anyone whose immune defenses are significantly weakened is at high risk. This includes people undergoing cancer chemotherapy, individuals who have received an organ transplant and are on anti-rejection medications, and those with conditions like HIV/AIDS.
- People with Certain Underlying Medical Conditions: The presence of other serious health issues can increase susceptibility. This includes individuals with advanced kidney disease, liver disease, or poorly controlled diabetes, as these conditions compromise the body's overall ability to mount a strong defense against infection.