What is Non-tuberculous Mycobacterial Infections?
Non-tuberculous mycobacterial (NTM) infections are illnesses resulting from a large and diverse group of bacteria naturally present in soil, dust, and water systems. These organisms belong to the same family as the bacterium responsible for tuberculosis, but they represent distinct species that do not cause that specific disease. NTM bacteria are considered opportunistic pathogens, meaning they typically only cause illness in susceptible individuals.
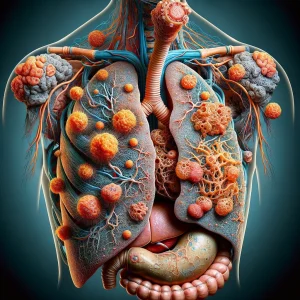
The most frequent presentation is pulmonary NTM disease, where the bacteria colonize and damage the lungs, often leading to inflammation and the formation of nodules or cavities. While the lungs are the primary target, NTM can sometimes cause infections in other parts of the body, such as the skin, soft tissues, or lymph nodes, particularly in people with severely compromised immune systems. The most common group of bacteria causing pulmonary NTM disease is the Mycobacterium avium complex (MAC).
Causes:- Environmental Exposure: The fundamental cause is direct contact with NTM bacteria, which are abundant in the natural world. They thrive in water sources like lakes and rivers, as well as in soil, household dust, and municipal water supplies.
- Inhalation of Aerosolized Bacteria: For pulmonary NTM, the most common form, the infection begins when a person breathes in microscopic droplets of water or particles of dust that contain the bacteria. Common sources of these aerosols include showerheads, hot tubs, and indoor swimming pools.
- Formation of Biofilms: NTM bacteria are adept at creating biofilms, which are slimy, protective layers that allow them to stick to surfaces. These biofilms frequently form inside plumbing pipes and fixtures, creating a persistent reservoir from which bacteria can be released into the water stream.
- Breach of Physical Barriers: In non-pulmonary cases, the infection can be initiated when the bacteria enter the body through a break in the skin, such as a cut or scrape, or during a surgical procedure with contaminated instruments.
- Underlying Structural Lung Conditions: The presence of pre-existing lung damage significantly increases vulnerability. Conditions such as bronchiectasis, which involves permanently widened and damaged airways, or Chronic Obstructive Pulmonary Disease (COPD), prevent the effective clearance of mucus and trapped particles, allowing NTM to colonize.
- Weakened Immune Defenses: Any condition or treatment that suppresses the immune system raises the risk of NTM infection. This includes individuals with autoimmune disorders, those taking immunosuppressant medications after an organ transplant, and people undergoing chemotherapy.
- Certain Physical Traits: A particular risk profile has been identified, especially in postmenopausal women, that includes a slender body build, scoliosis (curvature of the spine), or a concave chest wall (pectus excavatum). These characteristics can alter the anatomy of the chest cavity and affect how the lungs function.
- Tobacco Use: Smoking directly damages the lung's natural defense mechanisms, including the cilia, which are tiny hair-like structures responsible for sweeping out debris. This impairment makes it easier for inhaled NTM bacteria to establish a foothold.