What is Proctitis?
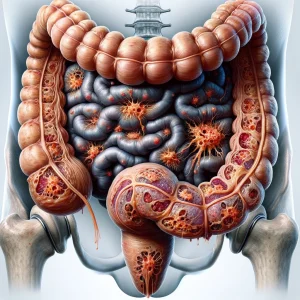
Proctitis is an inflammation isolated to the mucosal lining of the rectum. The rectum constitutes the final six inches of the large intestine, a muscular passage that extends from the end of the colon down to the anus. This condition involves the rectal tissue becoming swollen, reddened, and irritated.
As a result of this inflammation, the affected lining can become fragile and prone to bleeding or the formation of open sores, known as ulcers. Proctitis can be classified by its duration, presenting as an acute, short-lived episode or as a chronic, long-term condition. It is also categorized by its origin, which generally falls into either infectious or non-infectious types.
Causes:- Inflammatory Bowel Disease (IBD): Proctitis frequently arises as a direct manifestation of IBD. In conditions like ulcerative colitis and Crohn's disease, the body's immune system mistakenly attacks the gastrointestinal tract, and the rectum is a common site for this inflammatory assault.
- Infections from Pathogens: The introduction of certain infectious organisms into the rectum is a primary cause. This includes sexually transmitted infections (STIs), such as gonorrhea, chlamydia, and herpes, which can directly colonize the rectal lining through sexual contact. In addition, bacteria responsible for food poisoning, including Salmonella or Campylobacter, can lead to rectal inflammation.
- Complication from Radiation Therapy: Damage from medical treatments can induce the condition. Specifically, radiation therapy directed at pelvic cancers (like prostate or cervical cancer) can unintentionally expose the nearby rectum to radiation, injuring its lining and causing what is known as radiation proctitis.
- Disruption of the Gut Microbiome: The use of certain broad-spectrum antibiotics can alter the delicate balance of bacteria in the gut. This can allow harmful bacteria, such as Clostridioides difficile, to overgrow and release toxins that severely irritate the rectal tissue.
- Diversion Proctitis: This specific type can occur after a surgical procedure, such as a colostomy, that diverts the flow of stool away from the rectum. The absence of the fecal stream deprives the cells of the rectal lining of essential nutrients, leading to inflammation.
- Individuals with Inflammatory Bowel Disease: Anyone with a pre-existing diagnosis of Crohn's disease or ulcerative colitis has a significantly elevated risk, as rectal inflammation is a common feature of these chronic conditions.
- Patients Undergoing Pelvic Radiation: People receiving radiation treatment for cancers in the pelvic region, such as those affecting the prostate, cervix, or rectum itself, are susceptible to developing radiation-induced proctitis.
- Those Engaging in Anal Intercourse: The practice of receptive anal intercourse is a major risk factor for acquiring sexually transmitted infections that are known to directly cause infectious proctitis.
- Individuals with Compromised Immunity: A weakened immune system, whether from conditions like HIV/AIDS or from taking immunosuppressant medications, lowers the body's ability to fight off infections that can lead to proctitis.
- People with a Recent History of Antibiotic Therapy: Undergoing a course of strong antibiotics can disrupt the normal gut flora, placing a person at risk for opportunistic bacterial overgrowth and subsequent rectal inflammation.